The Liver Life Project
Stages of Liver Disease


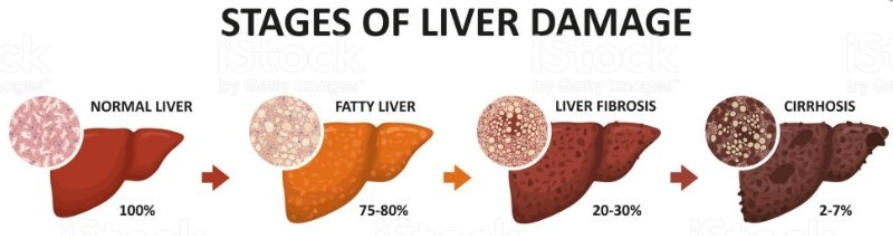

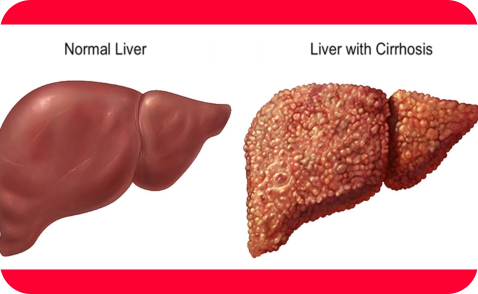
Cirrhosis is the result of long-term, continuous damage to the liver and may be due to many different causes. The damage leads to scarring, known as fibrosis. Irregular bumps
(nodules) replace the smooth liver tissue and the liver becomes harder. Together, the scarring and the nodules are called cirrhosis. Cirrhosis can take many years to develop and can
do so without any noticeable symptoms until the damage to the liver is very serious. The build-up of scar tissue can interfere with the flow of blood to your liver and stop it from
functioning properly. Cirrhosis can lead to liver failure.
How common is cirrhosis?
No one knows for sure how many people in the UK have cirrhosis as
most people do not know they have it until the condition becomes
serious. However, there is no doubt that the number of people with
the condition continues to increase. Every year over 4,000 people in
the UK die from cirrhosis and round 700 people have to have a liver
transplant each year to in order to survive.
Who is at risk of cirrhosis?
Cirrhosis can affect anyone – men and women, young and old.
People most at risk of cirrhosis:
1. Drink too much alcohol
2. Have a long-term liver infection, such as Hepatitis B or Hepatitis C
3. Have inherited liver disease, such as Haemochromatosis or
Alpha-1 Antitrypsin Deficiency (Alpha-1)
4. Have an immune system problem that leads to liver disease
5. Are clinically overweight or obese and have a fatty liver
Alcohol and cirrhosis
Almost everyone who drinks too much alcohol will suffer some liver damage, but this does not necessarily turn into cirrhosis. As many as nine out of ten people who drink to excess
will develop a fatty liver, with one in ten progressing to cirrhosis. In general, the more you drink, the greater your chance of developing alcohol-related hepatitis or cirrhosis. A poor
diet may make the problem much worse. Obesity is now the second biggest cause of Cirrhosis in the UK. All types of alcoholic drinks can lead to liver disease. If you have liver cirrhosis
whether it is caused by alcohol or not – you should not drink alcohol at all.
The Healthy Liver
The liver is our largest internal organ and it has 500 different roles and functions, including the breakdown of food into energy and helping the body get rid of waste products and fight infections - particularly in the bowel. And yet, when your liver is damaged, you generally won’t know about it – until things start to get serious. This is because the liver doesn’t have any pain receptors. Liver functions include: 1. Processing digested food from the intestine 2. Controlling levels of fats, amino acids and glucose in the blood 3. Combating infections 4. Clearing the blood of particles and infections, including bacteria 5. Neutralising and destroying all drugs and toxins 6. Manufacturing bile 7. Storing iron, vitamins and other essential chemicals 8. Breaking down food and turning it into energy 9. Manufacturing, breaking down and regulating numerous hormones including sex hormones 10. Making enzymes and proteins which are responsible for most chemical reactions in the body, for example those involved in blood clotting and repair of damaged tissues. Liver functions: The liver is one of five vital organs, which means it is necessary to keep you alive. The other vital organs are the brain, heart, lungs, and kidneys. Amazingly, only one third of your liver is needed to maintain normal functioning! This organ performs over five hundred vital tasks, and this video will discuss some of the most important ones! The liver is the human body’s second heaviest organ! It has four lobes - right, left, caudate, and quadrate. These lobes contain 1 million hexagonally-shaped hepatic lobules. Lobules are the functional unit of the liver, meaning that they are the smallest structures capable of performing the liver’s tasks. Lobules are made up of hepatocytes. A key task of the liver is to filter blood. At any given time, the liver contains 13% of your blood volume. Freshly oxygenated blood comes down from the heart’s aorta and enters the left and right hepatic arteries to supply the liver. Blood leaves the liver by the hepatic vein and goes through the inferior vena cava back to the heart. Then, circulation starts anew! The liver also receives blood through the portal vein from the gastrointestinal tract. It filters this blood to remove pathogens and toxins like alcohol and drugs. The liver and kidneys are the only “detox” your body will ever need! The filtered blood leaves the liver via the hepatic vein! The liver filters more than just toxins. It also houses Kupfer cells, which are a kind of immune cell called a tissue macrophage. Kupfer cells make up 80-90% of the body’s tissue macrophages! Kupfer cells remove and destroy old, or senescent, red blood cells. Red blood cells live for around 120 days before this happens. Kupffer cells destroy red blood cells through phagocytic action, and the hemoglobin within them gets recycled. Kupffer cells also destroy pathogens, which can enter through the portal vein. They sense bacteria or endotoxins, which are toxic substances bound to the bacterial cell wall and released when the bacterium ruptures or disintegrates. Upon detection, the Kupffer cells attack, releasing cytokines, nitric oxide, and oxygen species to destroy the pathogens! The Fatty Liver Except for the brain, the liver is the most complex organ in the body. Its functions include: 1. Filtering toxins from the blood 2. Aiding digestion of food 3. Regulating blood sugar and cholesterol levels 4. Helping to fight infection and disease The liver is very resilient and capable of regenerating itself. Each time your liver filters alcohol, some of the liver cells die. The liver can develop new cells, but prolonged alcohol misuse (drinking too much) over many years can reduce its ability to regenerate. This can result in serious and permanent damage to your liver. ARLD (Alcohol-related liver disease) is very common in the UK – the number of people with the condition has been increasing over the last few decades as a result of increasing levels of alcohol misuse. Drinking a large amount of alcohol, even for just a few days, can lead to a build-up of fats in the liver. This is called alcoholic fatty liver disease, and is the first stage of ARLD. The fatty liver disease rarely causes any symptoms, but it's an important warning sign that you're drinking at a harmful level. Fatty liver disease is reversible. If you stop drinking alcohol for two weeks, your liver should return to normalThe Liver Fibrosis
Fibrosis occurs when excessive scar tissue builds up faster than it can be broken down and removed from the liver. Chronic infection with hepatitis C or hepatitis B virus (HCV or HBV), heavy alcohol consumption, toxins, trauma or other factors can all lead toliver fibrosis. Only in rare instances is liver fibrosis the primary problem; more often, it is secondary to some other liver disease such as cirrhosis. Normally, the body’s response to injury is the formation of scar tissue. In the case of fibrosis, the healing process goes haywire. When hepatocytes (functional liver cells) are injured due to a virus, alcohol, toxins, trauma or other factors, the immune system goes to work to repair the damage. During the fibrosis process, the injured hepatocytes cause substances to be released into the liver causing the build-up of the scar tissue. In the early stages of liver fibrosis, few people experience symptoms because the liver functions relatively well. Fibrosis is the initial stage of the formation of scar tissue in the liver. An individual may have no symptoms and live a normal, sometimes very active life, for decades, and remain unaware that he or she has liver disease. As scar tissue builds up, due to inflammation and the continuance of liver injury, it connects with existing scar tissue, which can eventually disrupt the metabolic functions of the liver. If the disease progresses, it can lead to cirrhosis, a condition in which the liver is severely scarred, its blood flow is restricted, and its ability to function is impaired. If poked, a healthy liver is very soft. A liver that has developed fibrosis is firmer, and if the condition progresses to cirrhosis, the liver can become almost rock-hard.

Liver Cirrhosis