Medical Consequences

(Warning, this video is rather graphic)
In people who have cirrhosis, high blood pressure in the veins that
carry blood from the intestines to the liver can cause many problems.
One such serious complication is that of portal hypertension. When
blood pressure increases in the portal vein system, veins in the
oesophagus, stomach, and rectum enlarge to accommodate blocked
blood flow through the liver. The presence of enlarged veins (varices)
usually causes no symptoms. (They may be found during an
endoscopy exam of the oesophagus.) About 50 to 60 out of 100 people
who have cirrhosis develop varices in the oesophagus.
Some people may feel that this video sequence is too graphic. For this, I make no apologies. This condition is going to happen to you if your liver becomes too badly
damaged. 50% of those people who have cirrhosis of the liver will suffer from varices.

In some people with a liver disorder, ascitic fluid leaks from the surface
of the liver and intestine and accumulates within the abdomen. A
combination of factors is responsible. They include the following:
*
Portal hypertension
*
Fluid retention by the kidneys
Alterations in various hormones and chemicals that regulate body fluids.
Also, albumin usually leaks from blood vessels into the abdomen.
Normally, albumin, the main protein in the blood, helps keep fluid from
leaking out of blood vessels. When albumin leaks out of blood vessels,
fluid also leaks out.
A person with portal hypertension may also develop a build-up of fluid in their abdomen (tummy) and around the intestines. This fluid is known as Ascites. Initially,
this can be treated with water tablets (diuretics). If the problem progresses, many litres of fluid can build up, which needs to be drained. This is a procedure known
as Paracentesis involves a long, thin tube being placed into the fluid through the skin under
local anaesthetic
. One of the problems associated with the development
of ascites is the risk of infection in the fluid (spontaneous bacterial
peritonitis
). This is a potentially very serious complication and is linked to an increased risk of
kidney failure and death.
The main symptom of ascites is a swollen tummy. Other symptoms include:
pain and discomfort in the tummy
feeling sick (nausea)
reduced appetite
indigestion
feeling full
tiredness
breathlessness
Ascites can make it difficult for you to get comfortable, sit up and walk.








Hepatic encephalopathy is a brain disorder and refers to the changes in the brain that occur in patients with advanced,
acute or chronic liver disease and is one of the major complications of cirrhosis. Hepatic encephalopathy (HE) may
occur suddenly in people with acute liver failure; however, the condition is more often seen in people with chronic liver
disease.
An important job of the liver is to change harmful substances that are either made by the body or taken into the body
(such as medicines) and make them harmless. However, when the liver is damaged and unable to function fully, these
“toxins” may build up in the bloodstream. HE occurs when the liver cannot remove chemicals, such as ammonia. These chemicals then enter the brain and can
affect both the mental and physical condition of patients. Often, certain factors can be responsible for triggering an episode of HE in liver patients. The following
factors may trigger an episode of HE:
• Dehydration (loss of water from the body)
• Low oxygen levels in the body
• Eating too much protein
• Constipation
• Infections
• Intestine, stomach, or oesophagus bleeding
• Medications that affect the nervous system, such as tranquilisers
or sleep medications
• Kidney problems or Surgery
Patients with acute liver disease, who have an episode of HE, generally find that once the trigger is removed and their liver condition is treated, the HE disappears.
However, some patients with chronic liver disease find they will have recurring episodes of HE. Episodes of HE usually result in hospitalisation, as without
treatment, patients remain at high risk for recurrence. Other complications of untreated HE can be brain swelling, permanent nervous system damage, increased
risk of heart failure, kidney failure, respiratory failure and sepsis (blood poisoning) and in severe cases, coma.
HE symptoms can present at a range of stages from mild to overt (severe). Mild Symptoms of HE can be observed in nearly 70% of patients with cirrhosis. Overt HE
occurs in about 30-45% of patients with cirrhosis. HE symptoms can vary from person to person; they can develop rapidly or slowly over time. Patients with HE can
have both physical symptoms and reduced mental function.
I believe that it is so important for family members and friends to understand that when a person suffers from a HE episode. It isn’t the individual being mean or
nasty. It is a chemical reaction within the brain that is causing this uncommon behaviour. It isn’t the fault of the patient, and although the words are spoken and
often confusing, there is no real meaning behind them as they are being chemically driven.


For me, this is a thorny subject. Over the years, I’ve come across several diabetic nurses who, for some reason, seem to
once again put all type-2 diabetes sufferers in the same little box, and label everyone with the same condition and
cause.“
It’s because your pancreas isn’t producing enough insulin
”. This then blames the poor pancreas, when in truth it’s
having to work flat out.
I have carried out a lot of my research into the possible cause of my diabetes, and while I tend to avoid a lot of the American websites, I must confess that a huge
amount of research has been done into Type 2 Diabetes and liver disease by our esteemed cousins. It makes perfect sense to me that when the liver becomes
damaged through scarring or alcohol-related liver disease. Strange things will start to happen.
This is my understanding of what is going on:
The Liver is one of the most complicated organs in the body, and possibly the least understood. It plays a huge role in handling sugars and starches, making sure our
bodies have enough fuel to function. When there’s a lot of sugar in the system, it stores some of the excess in a storage form of carbohydrate called glycogen.
When blood sugar levels get low, as in times of hunger or at night, it converts some of the glycogen to glucose and makes it available for the body to use.
Easy to say, but how does the liver know what to do and when to do it? Scientists have found a “molecular switch” called the “CRTC2 gene” (or “Switch Gene” as
it’s sometimes called) that controls this process.
When the CRTC2 switch is on, the liver pours sugar (glucose) into the system. When there’s enough glucose circulating, CRTC2 should be turned off. The turn-off
signal is thought to be insulin. This may be an over
simplification
, though.
In a post-transplant patient, the medications used to prevent rejection can alter the way hepatocytes in the liver handle sugars and can drive the overproduction and
release of glucose into the blood. Also, patients with a diabetic risks before transplant are more likely to experience it after transplant. The other wonderful aspect of
this CRTC2 switch gene is that during a person’s REM sleep pattern, any excess sugars stored in the liver are burned off and
exhaled
through the lungs.
So, the CRTC2 gene does indeed act as a switch to produce more sugar in fasting situations and is down-regulated when abundant sugar is present. Levels change in
type 2 diabetes, and this makes the hyperglycemia worse. What’s most interesting is that the signals that act through this molecule are linked to a protein called
calcineurin, which is activated and causes the liver to make more sugar. The calcineurin levels increase in insulin-resistant states. CRTC2 is found in many cells,
including immune cells, heart and placenta, and some studies suggest in liver cells too. It is also down-regulated in some cancers.
However, calcineurin is also found in immune cells and is linked to growth and functional responses. So, some types of anti-rejection medications used after
transplant target calcineurin to dampen down anti-graft immune responses. Tacrolimus and cyclosporin are calcineurin inhibitors. We can therefore see how there
might be a connection between anti-rejection medication and the function of CRTC2.


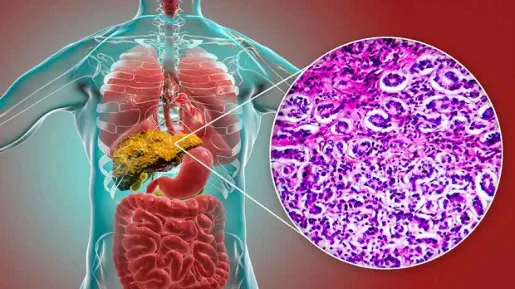
The human body is composed of billions of cells that are continually ageing, dying and being
replaced. Cell death, replacement, growth and development are normally tightly controlled. If
this control breaks down, cells begin to grow and divide abnormally, clustering together to
form a lump known as a tumour. These tumours are either benign or malignant. Cancer is the
name given to a malignant tumour. There are two broad categories of liver cancer: secondary
and primary.
1
.
Secondary liver cancer is cancer that first develops elsewhere in the body and
then spreads (metastasises) to the liver. It is sometimes called metastatic cancer.
2.
Primary liver cancers are cancers that start in the liver. The two main types are:
Hepatoma, also called hepatocellular carcinoma (HCC) and Biliary tree cancer, which includes cholangiocarcinoma (bile duct cancer) and
gallbladder cancer.
The Liver Life Project
Medical Consequences


I’ve been trolling the internet to find a suitable presentation of this
procedure, but sadly, there appears to be nothing available from a
British perspective. I have therefore used a
video taken from the
Barcelona Hospital Universitario to best illustrate this procedure.
I suspect the procedure to be pretty much the same.
This procedure does look a little tricky. I think the best way of
describing what TIPSS is, is to explain what each of the letters
stands for:
T.
Is for TRANSJUGULAR. This means that the radiologist will put a
fine, hollow needle into the jugular vein in your neck while you are
asleep. Through this needle, he or she will pass a fine, thin wire in a straight line until it reaches the veins from your liver. This is much easier than you would
imagine. Over this wire, the radiologist will pass a fine plastic tube called a catheter, about the size of a very long piece of spaghetti.
I.
Is for INTRAHEPATIC. The catheter that the radiologist has inserted will be passed down one of your liver veins into the liver itself. The radiologist will then take
the wire out and insert a long-curved needle.
PS.
is for PORTO-SYSTEMIC. The long needle will be pushed from your liver vein (or SYSTEMIC vein) into your PORTAL vein, which lies close to it. It is this portal
vein which has become partially blocked by your liver disease. Because of the blockage, there is high blood pressure in this part of your circulation, and this
procedure is designed to relieve this.
S.
is for SHUNT. Once the needle has been passed between your liver vein and the portal vein, a wire will be passed through the needle, and the needle will be
withdrawn. Over the wire, the radiologist will pass a metal spring called a stent. This stent will expand to create a channel between the two veins. Blood will then
flow from the high-pressure portal vein into the low-pressure liver (or systemic) vein. The high pressure in the portal vein, which is causing your problem, will
consequently be reduced back towards normal.
Using heat to destroy Cancer/Tumour cells (Ablation)
Ablation uses heat to destroy cancer cells.
Three types of ablation produce heat in different ways.
These are:
• Microwave
• Radiofrequency
• Laser ablation.
Each type destroys cancer cells by heating them to a high temperature. They may be used if you have
previously had surgery, or if you’re not fit enough to have surgery.
You will be given a sedative drug to make you feel drowsy and a local anaesthetic to numb the skin of your abdomen. Sometimes ablation is performed using a
general anaesthetic. The doctor puts a fine needle through the skin over your liver and into the centre of each tumour. An ultrasound or CT scan is used to guide
them. The microwave, radio-frequency or laser then produces heat which passes through the needle and into the tumour. This treatment takes about
30–60 minutes and can be used to treat tumours up to 5cm (2in) in size. You can usually go home a few hours after you’ve had your treatment.
The side effects of ablation are usually mild and may last up to a week. They include pain in the liver area, which you can
control by taking regular painkillers.
Other side effects are a fever (high temperature) and feeling tired and generally unwell. These side effects are due to the body getting rid of the cells that have
been destroyed. Try to drink plenty of fluids and get
enough rest. Your doctor or nurse may ask you to contact the hospital if your temperature doesn’t settle
within a few days or
if it goes higher than 38˚C (100.4°F). This is to make sure you don’t have an infection.
Your specialist can give you more information about the possible benefits and risks of these procedures. There is a useful guide from Southampton University
Hospital that may be of interest is at the following web address:
https://www.uhs.nhs.uk/Media/UHS-website-
2019/Patientinformation/Cancercare/Having-a-microwave-ablation-of-the-liver-2103-PIL.pdf

Normally, the blood from your gut returns in veins via the liver to the heart. The largest of these veins is called the Portal Vein. Due to the disease in your liver, there
is
increased
pressure
in
your
blood
vessels.
This
means
the
blood
struggles
to
flow
through
them
and
is
forced
to
find
alternative
routes
to
reach
your
heart.
One
of
these routes uses the veins in the bottom of your gullet. These veins start to carry more blood and become enlarged, leaky and can bleed easily. These distended
veins are called varices. If the varices start to bleed, this can lead to a very dangerous loss of blood.
The
distended
and
bleeding
vein
can
be
prevented
from
bursting
by
placing
an
elastic
type
of
band
over
it.
If
this
operation
does
not
control
the
bleeding,
your
doctor may have to consider other alternatives to reduce the pressure, such as a TIPSS procedure.
TIPSS (Transjugular Intrahepatic PortoSystemic Shunt)
I felt that the subject of “Alcohol-Induced Cancer” was too big a subject to be included here. I have therefore addressed this subject on a separate page.